Transplant Immunology
Transplantation is the process of moving cells, tissues, or organs, from one site to another, either within the same person or between a donor and a recipient. If an organ system fails, or becomes damaged as a consequence of disease or injury, it can be replaced with a healthy organ or tissue from a donor. Organ transplantation is a major operation and is only offered when all other treatment options have failed. Consequently, it is often a life-saving intervention. In 2015/16, 4,601 patient lives were saved or improved in the UK by an organ transplant.i Kidney transplants are the most common organ transplanted on the NHS in the UK (3,265 in 2015/16), followed by the liver (925), and pancreas (230).i In addition, a total of 383 combined heart and lung transplants were performed, while in 2015/16. However, whole organs are not the only type of transplant. The cornea, for example, is the most transplanted single tissue, with 5,734 procedures carried out in 2015/16.i Hematopoietic stem cell transplantation (HSCT), often called blood and marrow transplantation (BMT), is another common tissue transplantation procedure. Used to treat a broad spectrum of diseases, though most commonly for blood or bone marrow cancers such as leukaemia and lymphoma, around 3,600 HSCT transplants were undertaken in 2012.
The immune system plays a critical role in transplantation. The complex mechanisms of immunity, which under normal circumstances work to identify foreign microbes and direct the immune system to destroy them, pose a significant barrier to successful transplantation. Rejection of a transplant occurs in instances where the immune system identifies the transplant as foreign, triggering a response that will ultimately destroy the transplanted organ or tissue.
The intensity of the immune response against the organ or tissue, also commonly referred to as the graft, will depend on the type of graft being transplanted and the genetic disparity between the donor and recipient. To reduce the possibility of rejection, the donor and recipient are carefully matched for immune compatibility prior to transplantation. However, the small pool of eligible donors can make it difficult to find a donor-recipient match and there will always be a degree of rejection against the graft. A critical undersupply of donated organs means that waiting lists for transplants are extremely long. Patients needing a kidney transplantation, for example, wait on average 944 days (more than two and a half years) for a life-saving transplant.ii There were 6,943 patients registered for organ transplant in the UK as of March 2015.i Unfortunately, 479 of these patients died during 2015/16 whilst waiting for a transplant due the small pool of transplantable organs.i These figures underline the value of every organ and highlight the importance of a successful transplantation and maintaining long-term transplant survival. Manipulation of the immune system can support longterm survival of the graft ensuring that every transplant is as successful as possible.
There are several types of transplantation involving tissues and organs:
Autograft –Transplantation of cells, tissues or organs between sites within the same individual e.g. skin graft.
Allograft – Transplantation of organs or tissues from a donor to a non-genetically identical individual of the same species. Allografts are the most common type of transplant.
Xenograft – Transplantation of an organ or tissue between two different species. ‘Pig valves’, for example, are commonly used to repair or replace a defective heart valve in humans. In 2015/16, 6,069 xenograft valve replacements were carried out in England by the NHS.iii Xenotransplantation of whole organs is not currently viable, although it is an area of huge scientific interest as a potential solution for the existing critical undersupply of adequate organs.
ABO incompatible – ABO refers to blood group, which can vary between individuals. For most transplant types, matching of blood group between donor and recipient is a key strategy in reducing rejection risk. However, blood group compatibility is not always required for transplantations. For example, in the case of very young children with immature immune systems, ABO incompatible transplants can be carried out with less risk of transplant rejection.
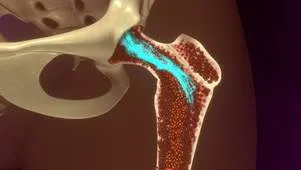
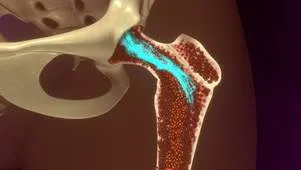
Stem cell transplant – Stem cells are cells that have the capacity to develop into a range of different types of cells in the body. Blood stem cells (haematopoietic stem cells) can develop into all the different cells found in the blood and are donated to replace damaged or destroyed blood cells. Haematopoietic stem cell transplants are used to treat certain types of cancer e.g. leukaemia, and blood diseases where the bone marrow has become damaged preventing the production of healthy blood cells. These stem cells can be harvested either directly from bone marrow (see image on left) or from the cord blood (blood from the placenta and umbilical cord) from consenting mothers following childbirth.
Distinguishing between self and non-self
When the immune system encounters a foreign organism, it mounts an attack against it to protect the body from infection. To prevent an attack on our own cells and tissues (autoimmunity), the immune system must be able to differentiate between our own healthy tissues and foreign invaders.
Foreign invaders are presented to the immune system in the form of small molecules called antigens. Identification of these non-self antigens will trigger an immune response and will stimulate the production of antigen specific antibodies that mark infected cells for destruction by the immune system and help amplify the immune response. The Human Leukocyte Antigen (HLA) complex is a group of genes that encode the proteins responsible for identifying foreign agents to the immune system. These proteins are found on the surface of all cells and act as ‘self-markers’ telling the immune system not to trigger a response.
Each person will have their own specific set of HLA proteins, based upon their unique genetic make-up, that the immune system will have learned not to react to. Any cell not displaying these specific HLA proteins will be identified as ‘non-self’ by the immune system and will be treated as a foreign invader.
Mechanism of rejection
Graft rejection occurs when the recipient’s immune system attacks the donated graft and begins destroying the transplanted tissue or organ. The immune response is usually triggered by the presence of the donor’s own unique set of HLA proteins, which the recipient’s immune system will identify as foreign.
The degree of similarity between the HLA genes of the donor and recipient is known as histocompatibility; the more genetically compatible the donor and the recipient, the more tolerant the recipient’s immune system should be of the graft. However, unless the donor and recipient are genetically identical (e.g. as in identical twins) there will always be some degree of rejection. As well as nonself HLA proteins, other surface proteins on the donor graft can also be identified as a foreign antigen and illicit an immune response.
In some cases, a patient may experience something known as ‘graft versus host reaction’ where mature immune cells already present in the donor graft begin attacking the healthy cells of the recipient. Graft versus host reaction, where the donor graft is described as being “immune-competent” (i.e. capable of producing an immune response) is a particular risk with stem cell transplants (bone marrow transplant) and can also occur following blood transfusions.
Clinical stages of rejection
Hyperacute rejection
This occurs within minutes or hours after a transplantation and is caused by the presence of preexisting antibodies of the recipient, that match the foreign antigens of the donor, triggering an immune response against the transplant. These antibodies could have been generated as a result of prior blood transfusions, prior transplantations or multiple pregnancies. The antibodies react with cells in the blood vessels of the graft, causing blood clots to form, which will prevent blood supply from reaching the graft resulting in immediate rejection of the transplant.
Acute rejection
This occurs within the first 6 months after transplantation. Some degree of acute rejection will occur in all transplantations, except between identical twins. Recipients are most at risk in the first 3 months, but rejection can still occur at a later stage. Acute rejection is caused by the formation of antibodies following the detection of non-self antigens in the donated graft. If diagnosed early enough, acute rejection can be treated by suppressing the immune system and permanent damage to the graft can be avoided in some cases.
Chronic rejection
Repeated episodes of acute rejection can ultimately lead to chronic rejection of the graft and failure of the transplant. Chronic rejection commonly manifests as scarring of the tissue or organ which can occur months to years after acute rejection has subsided. At present, there is no cure for chronic rejection other than removal of the graft.
Rejection can be minimised by carefully matching the donor and recipient for compatibility prior to transplantation. The better matched the donor and recipient are the more successful the transplantation is likely to be. Compatibility between donor and recipient is assessed using a combination of tests, including:
ABO blood group compatibility – The donor and recipient are tested for compatible blood groups. This is the first test to be carried out as the transplant will be rapidly rejected if the blood groups do no match. In some transplants, for example young children and also bone marrow transplants, ABO compatibility is not a necessity.

Tissue typing – A blood sample is taken from the recipient to identify the HLA antigens present on the surface of the their cells to help find a histone compatible donor. The more alike the HLA types of the donor and recipient are the more likely a transplant will be successful. Family members, in particular siblings, are often the best HLA matches due to their genetic similarity.
Cross matching – Blood samples are taken from both the recipient and donor, and the cells of the donor are mixed with the blood serum of the recipient. If the recipient’s antibodies attack the donor cells, they are considered a positive match and transplantation will not be suitable due to increased risk of hyper-acute rejection.
Panel reactive antibody test – The blood serum of patients awaiting transplantation are tested for reactive antibodies against a random panel of cells. Previous exposure to foreign tissue, by blood transfusion, pregnancy or prior transplantations, are likely to increase the number of HLA antibodies in the blood. The more HLA antibodies present, the higher he panel reactive antibody (PRA) level denoted to the patient, and the greater the chance of graft rejection. If PRA levels are high, it may be more difficult to find a match and a higher dosage of immunosuppressive drugs may be required.
Serology screening – For patients undergoing stem cell transplantation they and their donor will undergo pre-transplant serology screening. This is undertaken to detect the immune status of both the donor and a potential recipient against a number of clinically significant infectious organisms, including viruses like HIV, Cytomegalovirus (CMV), and Epstein-Barr Virus (EBV), thus determining potential for re-infection or reactivation of the infection upon immunosuppression. Individuals are often matched according to the CMV and EBV status.
To reduce the risk of transplant rejection, patients are treated with immunosuppressive drugs that will dampen their immune response. Immunosuppressive drugs are given in two phases; an initial induction phase involving a high dose, and a later maintenance phase which involves using the drug in the long term at a lower dose.
The combination of drugs, and dosage given, will vary depending on the type of transplant and the chosen treatment regime. If a patient experiences an episode of acute rejection the drug combination is subject to change and the dosage is also likely to increase. Side effects can also cause alternative drugs to be used. Steroids, in the past, have been the most commonly used immunosuppressant drug. However, their use is being reduced due to the adverse side effects associated with them.
All current immunosuppressive drugs come with limitations. One of the major limitations of these drugs is immunodeficiency. As these immunosuppressive drugs are non-specific, they will reduce overall immune system function leaving patients susceptible to opportunistic infection. Additionally, many of these drugs are associated with adverse side effects, such as high blood pressure, impaired renal function, diabetes mellitus, and increased risk of cancer – to name just a few. Patients are required to take a large number of immunosuppressants each day for the rest of their lives, which can have a major impact on their health and lifestyle. A fine balance needs to be reached between suppressing immune function sufficiently to avoid rejection, preventing drug toxicity, and maintaining enough immune function to fight off disease.
As well as new immunosuppressive drugs, with increased specificity and fewer side effects, other new therapies could also one day greatly reduce, or entirely remove, the possibility of rejection.
Stem cells could have a major impact on transplantation in the future beyond their current use in treating blood disorders. Pluripotent stem cells have the capacity to mature into any cell in the body, and this ability can be harnessed to grow tissues and organs. Moreover, the discovery that other cell types can be induced to have stem cell capacities means that the cells used to make the tissue could come directly from the recipient themselves, thus circumventing the risk of rejection.
Another future approach is the manufacture of organ scaffolds using 3D printing and then growing stem cells around these scaffolds to artificially replicate the tissue being replaced. Bio-manufacturing of tissues and organs would not only reduce the risk of transplant rejection, if the patient’s own stem cells were used, but would also reduce the strain on the limited organ supply.
However, the UK national strategy for organ transplantation (‘Taking organ transplantation to 2020: a UK strategy’) states that advances in stem cell treatment are unlikely to have a significant impact on organ donation over the next decade. Therefore, improving currently available therapies and the discovery of novel immunosuppressive regimes remains at the forefront of transplant medicine research.
Improving compatibility testing between donor and recipient could also reduce the risk of transplant rejection and increase the longevity of the transplant. The better matched the donor and the recipient are, the more tolerant the recipient’s immune system will be to the transplanted organ or tissue. Additionally, a greater understanding of the disparity between the donor and recipient will better inform treatment strategies after transplantation and help avoid repeated episodes of acute rejection.
Immunological research has led to huge advancements in transplant medicine. However, immune rejection still remains the most formidable barrier to successful transplantation. Continued research is needed to find ways to alleviate the risk of rejection, improve diagnosis and maintain long term survival of the transplant; all of which would have a significant impact on the strained organ supply.