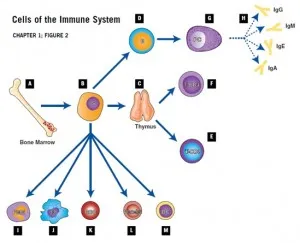
Cells of the Immune System
A. Bone marrow: The site in the body where most of the cells of the immune system are produced as immature or stem cells.
B. Stem cells: These cells have the potential to differentiate and mature into the different cells of the immune system.
C. Thymus: An organ located in the chest which instructs immature lymphocytes to become mature T-lymphocytes.
D. B-Cells: These lymphocytes arise in the bone marrow and differentiate into plasma cells which in turn produce immunoglobulins (antibodies).
E. Cytotoxic T-cells: These lymphocytes mature in the thymus and are responsible for killing infected cells.
F. Helper T-cells: These specialized lymphocytes “help” other T-cells and B-cells to perform their functions.
G. Plasma Cells: These cells develop from B-cells and are the cells that make immunoglobulin for the serum and the secretions.
H. Immunoglobulins: These highly specialized protein molecules, also known as antibodies, fit foreign antigens, such as polio, like a lock and key. Their variety is so extensive that they can be produced to match all possible microorganisms in our environment.
I. Neutrophils (Polymorphonuclear PMN Cell): A type of cell found in the blood stream that rapidly ingests microorganisms and kills them.
J. Monocytes: A type of phagocytic cell found in the blood stream which develops into a macrophage when it migrates to tissues.
K. Red Blood Cells: The cells in the blood stream which carry oxygen from the lungs to the tissues.
L. Platelets: Small cells in the blood stream which are important in blood clotting.
M. Dendritic Cells: Important cells in presenting antigen to immune system cells.
Components of the Immune System
Each major component of the immune system will be discussed separately below. Immune deficiencies can affect a single component or multiple components. The manifestations of immune deficiencies can be a single type of infection or a more global susceptibility to infection. Because of the many interactions between the cells and proteins of the immune system, some immune deficiencies can be associated with a very limited range of infections. For these immune deficiencies, there are other elements that “take up the slack” and can compensate at least partly for the missing piece. In other cases, the ability to defend against infection is very weak over all and the person may have significant problems with infections.
The cells of the immune system can be categorized as lymphocytes (T-cells, B-cells and NK cells), neutrophils, and monocytes/macrophages. These are all types of white blood cells. The major proteins of the immune system are predominantly signaling proteins (often called cytokines), antibodies, and complement proteins.
Lymphocytes of the Immune System
B-Cells
B-cells (sometimes called B-lymphocytes and often named on lab reports as CD19 or CD20 cells) are specialized cells of the immune system whose major function is to produce antibodies (also called immunoglobulins or gamma-globulins). B-cells develop in the bone marrow from hematopoietic stem cells. As part of their maturation in the bone marrow, B-cells are trained or educated so that they do not produce antibodies to healthy tissues. When mature, B-cells can be found in the bone marrow, lymph nodes, spleen, some areas of the intestine, and the bloodstream.
When B-cells encounter foreign material (antigens), they respond by maturing into another cell type called plasma cells. B-cells can also mature into memory cells, which allows a rapid response if the same infection is encountered again. Plasma cells are the mature cells that actually produce the antibodies. Antibodies, the major product of plasma cells, find their way into the bloodstream, tissues, respiratory secretions, intestinal secretions, and even tears. Antibodies are highly specialized serum protein molecules.
For every foreign antigen, there are antibody molecules specifically designed to fit that antigen, like a lock and key. For example, there are antibody molecules that physically fit the poliovirus, others that fit diphtheria, and still others that fit the measles virus. The variety of different antibody molecules is extensive so that B-cells have the ability to produce them against virtually all microbes in our environment. However, each plasma cell produces only one kind of antibody.
When antibody molecules recognize a microorganism as foreign, they physically attach to it and set off a complex chain of events involving other components of the immune system that work to eventually destroy the germ. Antibodies vary with respect to their specialized functions in the body. These variations are determined by the antibody’s chemical structure, which in turn determines the class of the antibody (or immunoglobulin).
There are five major classes of antibodies (IgG, IgA, IgM, IgD and IgE). IgG has four different subclasses (IgG1, IgG2, IgG3, IgG4). IgA has two subclasses (IgA1 and IgA2).
Each immunoglobulin class has distinct chemical characteristics that provide it with specific functions (Figure 3). For example, IgG antibodies are formed in large quantities, last in the circulation for a few weeks, and travel from the blood stream to the tissues easily. Only IgG crosses the placenta and passes some immunity from the mother to the newborn.
Antibodies of the IgA class are produced near mucus membranes and find their way into secretions such as tears, bile, saliva and mucus, where they protect against infection in the respiratory tract and intestines. Some of the IgA also appears in the circulation.
Antibodies of the IgM class are the first antibodies formed in response to infection. They are important in protection during the early days of an infection.
Antibodies of the IgE class are responsible for allergic reactions.
Antibodies protect the body against infection in a number of different ways. For example, some microorganisms, such as viruses, must attach to body cells before they can cause an infection, but antibodies bound to the surface of a virus can interfere with the virus’ ability to attach to the host cell. In addition, antibodies attached to the surface of some microorganisms can cause the activation of a group of proteins called the complement system that can directly kill some bacteria or viruses.
Antibody-coated bacteria are also much easier for neutrophils to ingest and kill than bacteria that are not coated with antibodies. All of these actions of antibodies prevent microorganisms from successfully invading body tissues and causing serious infections.
The long life of plasma cells enables us to retain immunity to viruses and bacteria that infected us many years ago. For example, once people have been fully immunized with live vaccine strains of measles virus, they will almost never catch it because they retain the plasma cells and antibodies for many years and these antibodies prevent infection.
T-Cells
T-cells (sometimes called T-lymphocytes and often named in lab reports as CD3 cells) are another type of immune cell. T-cells directly attack cells infected with viruses, and they also act as regulators of the immune system.
T-cells develop from hematopoietic stem cells in the bone marrow but complete their development in the thymus. The thymus is a specialized organ of the immune system in the chest. Within the thymus, immature lymphocytes develop into mature T-cells (the “T” stands for the thymus) and T-cells with the potential to attack normal tissues are eliminated. The thymus is essential for this process, and T-cells cannot develop if the fetus does not have a thymus. Mature T-cells leave the thymus and populate other organs of the immune system, such as the spleen, lymph nodes, bone marrow and blood.
Each T-cell reacts with a specific antigen, just as each antibody molecule reacts with a specific antigen. In fact, T-cells have molecules on their surfaces that are similar to antibodies. The variety of different T-cells is so extensive that the body has T-cells that can react against virtually any antigen.
T-cells have different abilities to recognize antigen and are varied in their function. There are “killer” or cytotoxic T-cells (often denoted in lab reports as CD8 T-cells), helper T-cells (often denoted in lab reports as CD4 T-cells), and regulatory T-cells. Each has a different role to play in the immune system.
Killer, or cytotoxic, T-cells perform the actual destruction of infected cells. Killer T-cells protect the body from certain bacteria and viruses that have the ability to survive and even reproduce within the body’s own cells. Killer T-cells also respond to foreign tissues in the body, such as a transplanted kidney. The killer cell must migrate to the site of infection and directly bind to its target to ensure its destruction.
Helper T-cells assist B-cells to produce antibodies and assist killer T-cells in their attack on foreign substances.
Regulatory T-cells suppress or turn off other T-lymphocytes. Without regulatory cells, the immune system would keep working even after an infection has been cured. Without regulatory T-cells, there is the potential for the body to “overreact” to the infection. Regulatory T-cells act as the thermostat of the lymphocyte system to keep it turned on just enough—not too much and not too little.