The Immune System
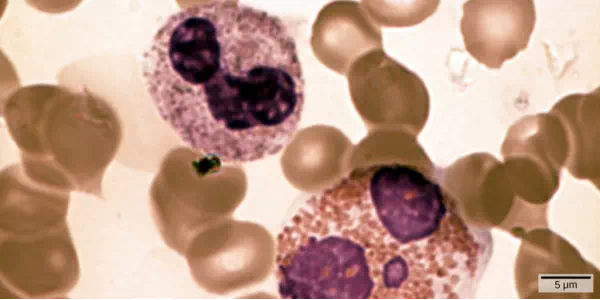
Figure 23.1. In this compound light micrograph purple-stained neutrophil (upper left) and eosinophil (lower right) are white blood cells that float among red blood cells in this blood smear. Neutrophils provide an early, rapid, and nonspecific defense against invading pathogens. Eosinophils play a variety of roles in the immune response. Red blood cells are about 7–8 µm in diameter, and a neutrophil is about 10–12µm. (credit: modification of work by Dr. David Csaba)
Introduction
The environment consists of numerous pathogens, which are agents, usually microorganisms, that cause diseases in their hosts. A host is the organism that is invaded and often harmed by a pathogen. Pathogens include bacteria, protists, fungi and other infectious organisms. We are constantly exposed to pathogens in food and water, on surfaces, and in the air. Mammalian immune systems evolved for protection from such pathogens; they are composed of an extremely diverse array of specialized cells and soluble molecules that coordinate a rapid and flexible defense system capable of providing protection from a majority of these disease agents.
Components of the immune system constantly search the body for signs of pathogens. When pathogens are found, immune factors are mobilized to the site of an infection. The immune factors identify the nature of the pathogen, strengthen the corresponding cells and molecules to combat it efficiently, and then halt the immune response after the infection is cleared to avoid unnecessary host cell damage. The immune system can remember pathogens to which it has been exposed to create a more efficient response upon re-exposure. This memory can last several decades. Features of the immune system, such as pathogen identification, specific response, amplification, retreat, and remembrance are essential for survival against pathogens. The immune response can be classified as either innate or active. The innate immune response is always present and attempts to defend against all pathogens rather than focusing on specific ones. Conversely, the adaptive immune response stores information about past infections and mounts pathogen-specific defenses.
Innate Immune Response
The immune system comprises both innate and adaptive immune responses. Innate immunityoccurs naturally because of genetic factors or physiology; it is not induced by infection or vaccination but works to reduce the workload for the adaptive immune response. Both the innate and adaptive levels of the immune response involve secreted proteins, receptor-mediated signaling, and intricate cell-to-cell communication. The innate immune system developed early in animal evolution, roughly a billion years ago, as an essential response to infection. Innate immunity has a limited number of specific targets: any pathogenic threat triggers a consistent sequence of events that can identify the type of pathogen and either clear the infection independently or mobilize a highly specialized adaptive immune response. For example, tears and mucus secretions contain microbicidal factors.
Physical and Chemical Barriers
Before any immune factors are triggered, the skin functions as a continuous, impassable barrier to potentially infectious pathogens. Pathogens are killed or inactivated on the skin by desiccation (drying out) and by the skin’s acidity. In addition, beneficial microorganisms that coexist on the skin compete with invading pathogens, preventing infection. Regions of the body that are not protected by skin (such as the eyes and mucus membranes) have alternative methods of defense, such as tears and mucus secretions that trap and rinse away pathogens, and cilia in the nasal passages and respiratory tract that push the mucus with the pathogens out of the body. Throughout the body are other defenses, such as the low pH of the stomach (which inhibits the growth of pathogens), blood proteins that bind and disrupt bacterial cell membranes, and the process of urination (which flushes pathogens from the urinary tract).
Despite these barriers, pathogens may enter the body through skin abrasions or punctures, or by collecting on mucosal surfaces in large numbers that overcome the mucus or cilia. Some pathogens have evolved specific mechanisms that allow them to overcome physical and chemical barriers. When pathogens do enter the body, the innate immune system responds with inflammation, pathogen engulfment, and secretion of immune factors and proteins.
Pathogen Recognition
An infection may be intracellular or extracellular, depending on the pathogen. All viruses infect cells and replicate within those cells (intracellularly), whereas bacteria and other parasites may replicate intracellularly or extracellularly, depending on the species. The innate immune system must respond accordingly: by identifying the extracellular pathogen and/or by identifying host cells that have already been infected. When a pathogen enters the body, cells in the blood and lymph detect the specific pathogen-associated molecular patterns (PAMPs) on the pathogen’s surface. PAMPs are carbohydrate, polypeptide, and nucleic acid “signatures” that are expressed by viruses, bacteria, and parasites but which differ from molecules on host cells. The immune system has specific cells, described in Figure 23.2 and shown in Figure 23.3, with receptors that recognize these PAMPs. A macrophage is a large phagocytic cell that engulfs foreign particles and pathogens. Macrophages recognize PAMPs via complementary pattern recognition receptors (PRRs). PRRs are molecules on macrophages and dendritic cells which are in contact with the external environment. A monocyte is a type of white blood cell that circulates in the blood and lymph and differentiates into macrophages after it moves into infected tissue. Dendritic cells bind molecular signatures of pathogens and promote pathogen engulfment and destruction. Toll-like receptors (TLRs) are a type of PRR that recognizes molecules that are shared by pathogens but distinguishable from host molecules). TLRs are present in invertebrates as well as vertebrates, and appear to be one of the most ancient components of the immune system. TLRs have also been identified in the mammalian nervous system.
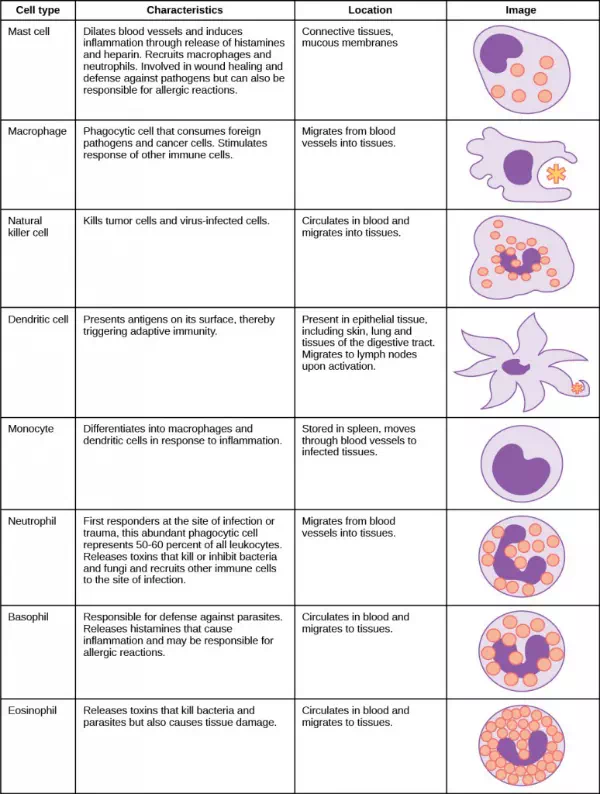
Figure 23.2. The characteristics and location of cells involved in the innate immune system are described. (credit: modification of work by NIH)
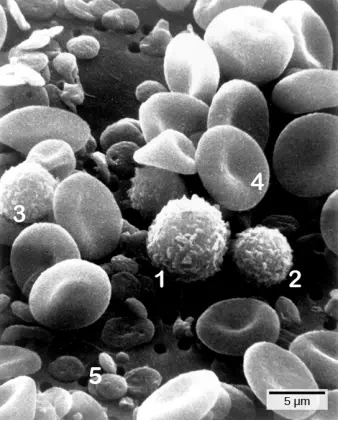
Figure 23.3. Cells of the blood include (1) monocytes, (2) lymphocytes, (3) neutrophils, (4) red blood cells, and (5) platelets. Note the very similar morphologies of the leukocytes (1, 2, 3). (credit: modification of work by Bruce Wetzel, Harry Schaefer, NCI; scale-bar data from Matt Russell)
Cytokine Release Affect
The binding of PRRs with PAMPs triggers the release of cytokines, which signal that a pathogen is present and needs to be destroyed along with any infected cells. A cytokine is a chemical messenger that regulates cell differentiation (form and function), proliferation (production), and gene expression to affect immune responses. At least 40 types of cytokines exist in humans that differ in terms of the cell type that produces them, the cell type that responds to them, and the changes they produce. One type cytokine, interferon, is illustrated in Figure 23.4.
One subclass of cytokines is the interleukin (IL), so named because they mediate interactions between leukocytes (white blood cells). Interleukins are involved in bridging the innate and adaptive immune responses. In addition to being released from cells after PAMP recognition, cytokines are released by the infected cells which bind to nearby uninfected cells and induce those cells to release cytokines, which results in a cytokine burst.
A second class of early-acting cytokines is interferons, which are released by infected cells as a warning to nearby uninfected cells. One of the functions of an interferon is to inhibit viral replication. They also have other important functions, such as tumor surveillance. Interferons work by signaling neighboring uninfected cells to destroy RNA and reduce protein synthesis, signaling neighboring infected cells to undergo apoptosis (programmed cell death), and activating immune cells.
In response to interferons, uninfected cells alter their gene expression, which increases the cells’ resistance to infection. One effect of interferon-induced gene expression is a sharply reduced cellular protein synthesis. Virally infected cells produce more viruses by synthesizing large quantities of viral proteins. Thus, by reducing protein synthesis, a cell becomes resistant to viral infection.
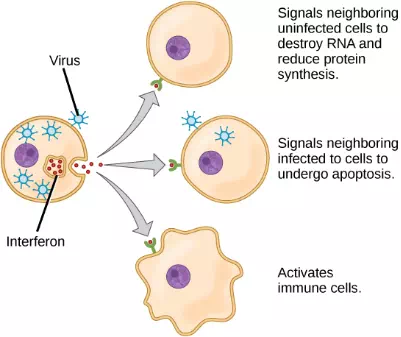
Figure 23.4. Interferons are cytokines that are released by a cell infected with a virus. Response of neighboring cells to interferon helps stem the infection.