Endocrine Glands
Both the endocrine and nervous systems use chemical signals to communicate and regulate the body’s physiology. The endocrine system releases hormones that act on target cells to regulate development, growth, energy metabolism, reproduction, and many behaviors. The nervous system releases neurotransmitters or neurohormones that regulate neurons, muscle cells, and endocrine cells. Because the neurons can regulate the release of hormones, the nervous and endocrine systems work in a coordinated manner to regulate the body’s physiology.
Hypothalamic-Pituitary Axis
The hypothalamus in vertebrates integrates the endocrine and nervous systems. The hypothalamus is an endocrine organ located in the diencephalon of the brain. It receives input from the body and other brain areas and initiates endocrine responses to environmental changes. The hypothalamus acts as an endocrine organ, synthesizing hormones and transporting them along axons to the posterior pituitary gland. It synthesizes and secretes regulatory hormones that control the endocrine cells in the anterior pituitary gland. The hypothalamus contains autonomic centers that control endocrine cells in the adrenal medulla via neuronal control.
The pituitary gland, sometimes called the hypophysis or “master gland” is located at the base of the brain in the sella turcica, a groove of the sphenoid bone of the skull, illustrated in Figure 18.15. It is attached to the hypothalamus via a stalk called the pituitary stalk (or infundibulum). The anterior portion of the pituitary gland is regulated by releasing or release-inhibiting hormones produced by the hypothalamus, and the posterior pituitary receives signals via neurosecretory cells to release hormones produced by the hypothalamus. The pituitary has two distinct regions—the anterior pituitary and the posterior pituitary—which between them secrete nine different peptide or protein hormones. The posterior lobe of the pituitary gland contains axons of the hypothalamic neurons.
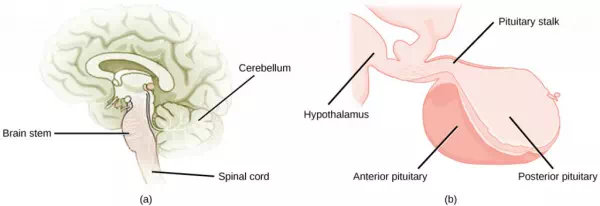
Figure 18.15. The pituitary gland is located at (a) the base of the brain and (b) connected to the hypothalamus by the pituitary stalk. (credit a: modification of work by NCI; credit b: modification of work by Gray’s Anatomy)
Anterior Pituitary
The anterior pituitary gland, or adenohypophysis, is surrounded by a capillary network that extends from the hypothalamus, down along the infundibulum, and to the anterior pituitary. This capillary network is a part of the hypophyseal portal system that carries substances from the hypothalamus to the anterior pituitary and hormones from the anterior pituitary into the circulatory system. A portal system carries blood from one capillary network to another; therefore, the hypophyseal portal system allows hormones produced by the hypothalamus to be carried directly to the anterior pituitary without first entering the circulatory system.
The anterior pituitary produces seven hormones: growth hormone (GH), prolactin (PRL), thyroid-stimulating hormone (TSH), melanin-stimulating hormone (MSH), adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), and luteinizing hormone (LH). Anterior pituitary hormones are sometimes referred to as tropic hormones, because they control the functioning of other organs. While these hormones are produced by the anterior pituitary, their production is controlled by regulatory hormones produced by the hypothalamus. These regulatory hormones can be releasing hormones or inhibiting hormones, causing more or less of the anterior pituitary hormones to be secreted. These travel from the hypothalamus through the hypophyseal portal system to the anterior pituitary where they exert their effect. Negative feedback then regulates how much of these regulatory hormones are released and how much anterior pituitary hormone is secreted.
Posterior Pituitary
The posterior pituitary is significantly different in structure from the anterior pituitary. It is a part of the brain, extending down from the hypothalamus, and contains mostly nerve fibers and neuroglial cells, which support axons that extend from the hypothalamus to the posterior pituitary. The posterior pituitary and the infundibulum together are referred to as the neurohypophysis.
The hormones antidiuretic hormone (ADH), also known as vasopressin, and oxytocin are produced by neurons in the hypothalamus and transported within these axons along the infundibulum to the posterior pituitary. They are released into the circulatory system via neural signaling from the hypothalamus. These hormones are considered to be posterior pituitary hormones, even though they are produced by the hypothalamus, because that is where they are released into the circulatory system. The posterior pituitary itself does not produce hormones, but instead stores hormones produced by the hypothalamus and releases them into the blood stream.
Thyroid Gland
The thyroid gland is located in the neck, just below the larynx and in front of the trachea, as shown in Figure 18.16. It is a butterfly-shaped gland with two lobes that are connected by the isthmus. It has a dark red color due to its extensive vascular system. When the thyroid swells due to dysfunction, it can be felt under the skin of the neck.
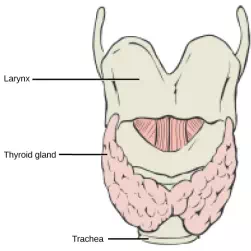
Figure 18.16. This illustration shows the location of the thyroid gland.
The thyroid gland is made up of many spherical thyroid follicles, which are lined with a simple cuboidal epithelium. These follicles contain a viscous fluid, called colloid, which stores the glycoprotein thyroglobulin, the precursor to the thyroid hormones. The follicles produce hormones that can be stored in the colloid or released into the surrounding capillary network for transport to the rest of the body via the circulatory system.
Thyroid follicle cells synthesize the hormone thyroxine, which is also known as T4 because it contains four atoms of iodine, and triiodothyronine, also known as T3 because it contains three atoms of iodine. Follicle cells are stimulated to release stored T3 and T4 by thyroid stimulating hormone (TSH), which is produced by the anterior pituitary. These thyroid hormones increase the rates of mitochondrial ATP production.
A third hormone, calcitonin, is produced by parafollicular cells of the thyroid either releasing hormones or inhibiting hormones. Calcitonin release is not controlled by TSH, but instead is released when calcium ion concentrations in the blood rise. Calcitonin functions to help regulate calcium concentrations in body fluids. It acts in the bones to inhibit osteoclast activity and in the kidneys to stimulate excretion of calcium. The combination of these two events lowers body fluid levels of calcium.
Parathyroid Glands
Most people have four parathyroid glands; however, the number can vary from two to six. These glands are located on the posterior surface of the thyroid gland, as shown in Figure 18.17. Normally, there is a superior gland and an inferior gland associated with each of the thyroid’s two lobes. Each parathyroid gland is covered by connective tissue and contains many secretory cells that are associated with a capillary network.
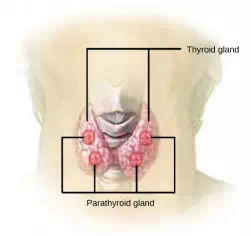
Figure 18.17. The parathyroid glands are located on the posterior of the thyroid gland. (credit: modification of work by NCI)
The parathyroid glands produce parathyroid hormone (PTH). PTH increases blood calcium concentrations when calcium ion levels fall below normal. PTH (1) enhances reabsorption of Ca2+by the kidneys, (2) stimulates osteoclast activity and inhibits osteoblast activity, and (3) it stimulates synthesis and secretion of calcitriol by the kidneys, which enhances Ca2+ absorption by the digestive system. PTH is produced by chief cells of the parathyroid. PTH and calcitonin work in opposition to one another to maintain homeostatic Ca2+ levels in body fluids. Another type of cells, oxyphil cells, exist in the parathyroid but their function is not known. These hormones encourage bone growth, muscle mass, and blood cell formation in children and women.
Adrenal Glands
The adrenal glands are associated with the kidneys; one gland is located on top of each kidney as illustrated in Figure 18.18. The adrenal glands consist of an outer adrenal cortex and an inner adrenal medulla. These regions secrete different hormones.
Pancreas
The pancreas, illustrated in Figure 18.19, is an elongated organ that is located between the stomach and the proximal portion of the small intestine. It contains both exocrine cells that excrete digestive enzymes and endocrine cells that release hormones. It is sometimes referred to as a heterocrine gland because it has both endocrine and exocrine functions.
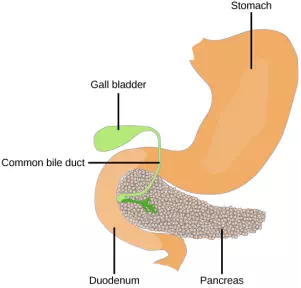
Figure 18.19. The pancreas is found underneath the stomach and points toward the spleen. (credit: modification of work by NCI)
The endocrine cells of the pancreas form clusters called pancreatic islets or the islets of Langerhans, as visible in the micrograph shown in Figure 18.20. The pancreatic islets contain two primary cell types: alpha cells, which produce the hormone glucagon, and beta cells, which produce the hormone insulin. These hormones regulate blood glucose levels. As blood glucose levels decline, alpha cells release glucagon to raise the blood glucose levels by increasing rates of glycogen breakdown and glucose release by the liver. When blood glucose levels rise, such as after a meal, beta cells release insulin to lower blood glucose levels by increasing the rate of glucose uptake in most body cells, and by increasing glycogen synthesis in skeletal muscles and the liver. Together, glucagon and insulin regulate blood glucose levels.
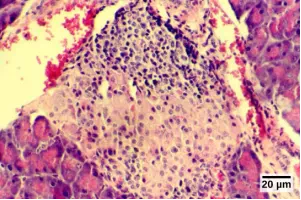
Figure 18.20. The islets of Langerhans are clusters of endocrine cells found in the pancreas; they stain lighter than surrounding cells.
Pineal Gland
The pineal gland produces melatonin. The rate of melatonin production is affected by the photoperiod. Collaterals from the visual pathways innervate the pineal gland. During the day photoperiod, little melatonin is produced; however, melatonin production increases during the dark photoperiod (night). In some mammals, melatonin has an inhibitory affect on reproductive functions by decreasing production and maturation of sperm, oocytes, and reproductive organs. Melatonin is an effective antioxidant, protecting the CNS from free radicals such as nitric oxide and hydrogen peroxide. Lastly, melatonin is involved in biological rhythms, particularly circadian rhythms such as the sleep-wake cycle and eating habits.
Gonads
The gonads—the male testes and female ovaries—produce steroid hormones. The testes produce androgens, testosterone being the most prominent, which allow for the development of secondary sex characteristics and the production of sperm cells. The ovaries produce estradiol and progesterone, which cause secondary sex characteristics and prepare the body for childbirth.
|
Table 18.1. |
||
|
Endocrine Glands and their Associated Hormones |
||
|
Endocrine Gland |
Associated Hormones |
Effect |
|
Hypothalamus |
releasing and inhibiting hormones |
regulate hormone release from pituitary gland; produce oxytocin; produce uterine contractions and milk secretion in females |
|
antidiuretic hormone (ADH) |
water reabsorption from kidneys; vasoconstriction to increase blood pressure |
|
|
Pituitary (Anterior) |
growth hormone (GH) |
promotes growth of body tissues, protein synthesis; metabolic functions |
|
prolactin (PRL) |
promotes milk production |
|
|
thyroid stimulating hormone (TSH) |
stimulates thyroid hormone release |
|
|
adrenocorticotropic hormone (ACTH) |
stimulates hormone release by adrenal cortex, glucocorticoids |
|
|
follicle-stimulating hormone (FSH) |
stimulates gamete production (both ova and sperm); secretion of estradiol |
|
|
luteinizing hormone (LH) |
stimulates androgen production by gonads; ovulation, secretion of progesterone |
|
|
melanocyte-stimulating hormone (MSH) |
stimulates melanocytes of the skin increasing melanin pigment production. |
|
|
Pituitary (Posterior) |
antidiuretic hormone (ADH) |
stimulates water reabsorption by kidneys |
|
oxytocin |
stimulates uterine contractions during childbirth; milk ejection; stimulates ductus deferens and prostate gland contraction during emission |
|
|
Thyroid |
thyroxine, triiodothyronine |
stimulate and maintain metabolism; growth and development |
|
calcitonin |
reduces blood Ca2+ levels |
|
|
Parathyroid |
parathyroid hormone (PTH) |
increases blood Ca2+ levels |
|
Adrenal (Cortex) |
aldosterone |
increases blood Na+ levels; increase K+ secretion |
|
cortisol, corticosterone, cortisone |
increase blood glucose levels; anti-inflammatory effects |
|
|
Adrenal (Medulla) |
epinephrine, norepinephrine |
stimulate fight-or-flight response; increase blood gluclose levels; increase metabolic activities |
|
Pancreas |
insulin |
reduces blood glucose levels |
|
glucagon |
increases blood glucose levels |
|
|
Pineal gland |
melatonin |
regulates some biological rhythms and protects CNS from free radicals |
|
Testes |
androgens |
regulate, promote, increase or maintain sperm production; male secondary sexual characteristics |
|
Ovaries |
estrogen |
promotes uterine lining growth; female secondary sexual characteristics |
|
progestins |
promote and maintain uterine lining growth |
|