Using Neural Tissue Engineering to Restore Brain Function and Form Bionic Connections
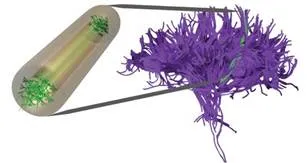
Restoring Brain Connections using Micro-Tissue Engineered Neural Networks (TENNs): Micro-TENNs are miniature preformed capsule-like constructs (shown above) that consist of neurons spanned by long axon tracts. These are grown outside the body and mimic the anatomy of axon pathways in the brain. They can then be implanted in the brain to physically reconstruct dysfunctional neural circuits
It is true that brain cells die easily, whether by drinking copious amounts of alcohol , through trauma, neurodegenerative disease, or even as a normal part of aging. In fact, that cell death process starts as soon as a newborn baby takes its first breaths.
“We have more brain cells at birth than we have at any point in our lives,” says D. Kacy Cullen, PhD, a research assistant professor in the department of Neurosurgery.
The brain is unique among organs. The function of nerve cells (neurons) gives rise to consciousness — who we are — yet these cells have very limited capacity to regenerate. Nerve cells work by growing long fibrous projections known as axons which connect neurons within the brain and form the body’s signal transmission and communication structure.
Although new neurons are born in select regions of the brain, the long axon cables crisscrossing the brain do not regenerate, yet they are necessary for normal function. Researchers have been working for decades to coax damaged axons to regenerate, with little success in getting enough axons to grow to the right places.
But, it turns out that groups of nerve cells, or tissue, can be organized outside the body and engineered to restore and repair axon pathways in the nervous system that may be damaged by injury or disease. Dr. Cullen is a national leader in the emerging area of research known as neural tissue engineering. He works at the intersection of neuroscience and engineering to come up with unique ways to aid those with brain function-related issues.
“Replacing individual cells does not work, but if we reform the tissue structure, complete with long axons, we are seeing signs that this engineered tissue will link into the existing tissue in the brain to mimic the function of the missing structures,” says Cullen.
The team has started to see success with this technology in testing in the lab.
“This is a great example of the promise of personalized medicine,” says Cullen. “In the not-too-distant future, our hope is that we can determine what neuronal and axonal structures a person is missing, grow a replacement to match the missing structure, and give them back the function that disease or injury took away.”
This technology holds great possibility for patients with neurodegenerative diseases, such as Parkinson’s and Alzheimer’s disease.
This technology also has promise to form bionic connections with the brain. Cullen has partnered with Brian Litt, MD, professor of Neurology and Bioengineering, and head of the new Penn Center for Neuroengineering and Therapeutics, to use these tissue engineering techniques as a biological link between man and machine.
Penn’s growing body of researchers in neural engineering and regenerative medicine will help make these breakthroughs someday translate into monumental advances for patients with brain injuries and brain disorders.