Menstrual Cycle
Menstruation is the shedding of the lining of the uterus (endometrium) accompanied by bleeding. It occurs in approximately monthly cycles throughout a woman's reproductive life, except during pregnancy. Menstruation starts during puberty (at menarche) and stops permanently at menopause.
By definition, the menstrual cycle begins with the first day of bleeding, which is counted as day 1. The cycle ends just before the next menstrual period. Menstrual cycles normally range from about 25 to 36 days. Only 10 to 15% of women have cycles that are exactly 28 days. Also, in at least 20% of women, cycles are irregular. That is, they are longer or shorter than the normal range. Usually, the cycles vary the most and the intervals between periods are longest in the years immediately after menstruation starts (menarche) and before menopause.
Menstrual bleeding lasts 3 to 7 days, averaging 5 days. Blood loss during a cycle usually ranges from 1/2 to 2 1/2 ounces. A sanitary pad or tampon, depending on the type, can hold up to an ounce of blood. Menstrual blood, unlike blood resulting from an injury, usually does not clot unless the bleeding is very heavy.
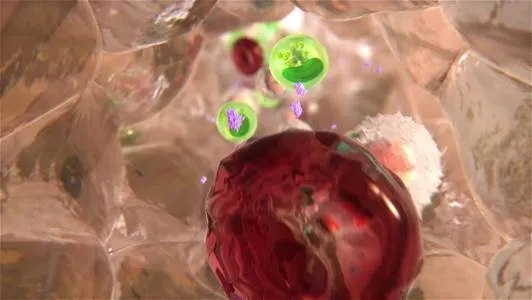
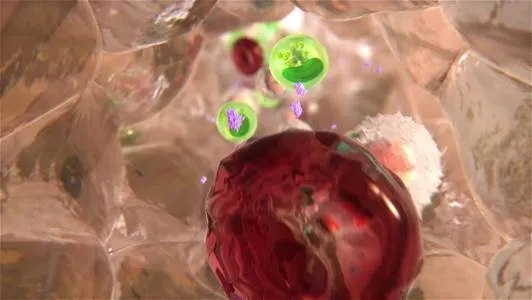
The menstrual cycle is regulated by hormones. Luteinizing hormone and follicle-stimulating hormone, which are produced by the pituitary gland, promote ovulation and stimulate the ovaries to produce estrogen and progesterone. Estrogen and progesterone stimulate the uterus and breasts to prepare for possible fertilization.
The Pituitary and Hypothalamus
The Testes and Ovaries

The menstrual cycle has three phases:
· Follicular (before release of the egg)
· Ovulatory (egg release)
· Luteal (after egg release)
Changes During the Menstrual Cycle
|
The menstrual cycle is regulated by the complex interaction of hormones: luteinizing hormone, follicle-stimulating hormone, and the female sex hormones estrogen and progesterone. The menstrual cycle has three phases:
The menstrual cycle begins with menstrual bleeding (menstruation), which marks the first day of the follicular phase. When the follicular phase begins, levels of estrogen and progesterone are low. As a result, the top layers of the thickened lining of the uterus (endometrium) break down and are shed, and menstrual bleeding occurs. About this time, the follicle-stimulating hormone level increases slightly, stimulating the development of several follicles in the ovaries. Each follicle contains an egg. Later in this phase, as the follicle-stimulating hormone level decreases, only one follicle continues to develop. This follicle produces estrogen. The ovulatory phase begins with a surge in luteinizing hormone and follicle-stimulating hormone levels. Luteinizing hormone stimulates egg release (ovulation), which usually occurs 16 to 32 hours after the surge begins. The estrogen level decreases during the surge, and the progesterone level starts to increase. During the luteal phase, luteinizing hormone and follicle-stimulating hormone levels decrease. The ruptured follicle closes after releasing the egg and forms a corpus luteum, which produces progesterone. During most of this phase, the estrogen level is high. Progesterone and estrogen cause the lining of the uterus to thicken more, to prepare for possible fertilization. If the egg is not fertilized, the corpus luteum degenerates and no longer produces progesterone, the estrogen level decreases, the top layers of the lining break down and are shed, and menstrual bleeding occurs (the start of a new menstrual cycle). If the egg is fertilized, the corpus luteum continues to function during early pregnancy. It helps maintain the pregnancy. |
The follicular phase begins on the first day of menstrual bleeding (day 1). But the main event in this phase is the development of follicles in the ovaries.
At the beginning of the follicular phase, the lining of the uterus (endometrium) is thick with fluids and nutrients designed to nourish an embryo. If no egg has been fertilized, estrogen and progesterone levels are low. As a result, the top layers of the endometrium are shed, and menstrual bleeding occurs.
About this time, the pituitary gland slightly increases its production of follicle-stimulating hormone. This hormone then stimulates the growth of 3 to 30 follicles. Each follicle contains an egg. Later in the phase, as the level of this hormone decreases, only one of these follicles (called the dominant follicle) continues to grow. It soon begins to produce estrogen, and the other stimulated follicles begin to break down. The increasing estrogen also begins to prepare the uterus and stimulates the luteinizing hormone surge.
On average, the follicular phase lasts about 13 or 14 days. Of the three phases, this phase varies the most in length. It tends to become shorter near menopause. This phase ends when the level of luteinizing hormone increases dramatically (surges). The surge results in release of the egg (ovulation) and marks the beginning of the next phase.
The ovulatory phase begins when the level of luteinizing hormone surges. Luteinizing hormone stimulates the dominant follicle to bulge from the surface of the ovary and finally rupture, releasing the egg. The level of follicle-stimulating hormone increases to a lesser degree. The function of the increase in follicle-stimulating hormone is not understood.
The ovulatory phase usually lasts 16 to 32 hours. It ends when the egg is released, about 10 to 12 hours after the surge in the level of luteinizing hormone. The egg can be fertilized for only up to about 12 hours after its release.
The surge in luteinizing hormone can be detected by measuring the level of this hormone in urine. This measurement can be used to determine when women are fertile. Fertilization is more likely when sperm are present in the reproductive tract before the egg is released. Most pregnancies occur when intercourse occurs within 3 days before ovulation.
Around the time of ovulation, some women feel a dull pain on one side of the lower abdomen. This pain is known as mittelschmerz (literally, middle pain). The pain may last for a few minutes to a few hours. The pain is usually felt on the same side as the ovary that released the egg, but the precise cause of the pain is unknown. The pain may precede or follow the rupture of the follicle and may not occur in all cycles.
Egg release does not alternate between the two ovaries and appears to be random. If one ovary is removed, the remaining ovary releases an egg every month.
The luteal phase begins after ovulation. It lasts about 14 days (unless fertilization occurs) and ends just before a menstrual period.
In this phase, the ruptured follicle closes after releasing the egg and forms a structure called a corpus luteum, which produces increasing quantities of progesterone. The progesterone produced by the corpus luteum does the following:
· Prepares the uterus in case an embryo is implanted
· Causes the endometrium to thicken, filling with fluids and nutrients to nourish a potential embryo
· Causes the mucus in the cervix to thicken, so that sperm or bacteria are less likely to enter the uterus
· Causes body temperature to increase slightly during the luteal phase and remain elevated until a menstrual period begins (this increase in temperature can be used to estimate whether ovulation has occurred)
During most of the luteal phase, the estrogen level is high. Estrogen also stimulates the endometrium to thicken.
The increase in estrogen and progesterone levels causes milk ducts in the breasts to widen (dilate). As a result, the breasts may swell and become tender.
If the egg is not fertilized or if the fertilized egg does not implant, the corpus luteum degenerates after 14 days, levels of estrogen and progesterone decrease, and a new menstrual cycle begins.
If the embryo is implanted, the cells around the developing embryo begin to produce a hormone called human chorionic gonadotropin. This hormone maintains the corpus luteum, which continues to produce progesterone, until the growing fetus can produce its own hormones. Pregnancy tests are based on detecting an increase in the human chorionic gonadotropin level.