Human blood
Blood Components
Normally, 7-8% of human body weight is from blood. In
adults, this amounts to 4.5-6 quarts of blood. This essential fluid
carries out the critical functions of transporting oxygen and nutrients to our
cells and getting rid of carbon dioxide, ammonia, and other waste
products. In addition, it plays a vital role in our immune system and in
maintaining a relatively constant body temperature. Blood is a highly
specialized tissue composed of more than 4,000 different kinds of
components. Four of the most important ones are red cells, white cells,
platelets, and plasma. All humans produce these blood components--there
are no populational or regional differences.
Red Cells
|
|
|
|
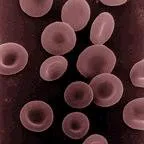
Human erythrocytes or "red
cells" |
Red cells, or erythrocytes , are relatively large microscopic cells without nuclei. In this latter trait, they are similar to the primitive prokaryotic cells of bacteria. Red cells normally make up 40-50% of the total blood volume. They transport oxygen from the lungs to all of the living tissues of the body and carry away carbon dioxide. The red cells are produced continuously in our bone marrow from stem cells at a rate of about 2-3 million cells per second. Hemoglobin is the gas transporting protein molecule that makes up 95% of a red cell. Each red cell has about 270,000,000 iron-rich hemoglobin molecules. People who are anemic generally have a deficiency in red cells, and subsequently feel fatigued due to a shortage of oxygen. The red color of blood is primarily due to oxygenated red cells. Human fetal hemoglobin molecules differ from those produced by adults in the number of amino acid chains. Fetal hemoglobin has three chains, while adults produce only two. As a consequence, fetal hemoglobin molecules attract and transport relatively more oxygen to the cells of the body.
White Cells
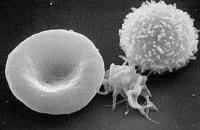
White cells, or leukocytes ,
exist in variable numbers and types but make up a very small part of blood's
volume--normally only about 1% in healthy people. Leukocytes are not
limited to blood. They occur elsewhere in the body as well, most notably in
the spleen, liver, and lymph glands. Most are produced in our bone marrow
from the same kind of stem cells that produce red blood cells. Others are
produced in the thymus gland, which is at the base of the neck. Some
white cells (called lymphocytes  ) are the first responders for our immune system. They seek
out, identify, and bind to alien protein on bacteria, viruses,
and fungi so that they can be removed. Other white cells
(called granulocytes and macrophages ) then arrive to
surround and destroy the alien cells. They also have the function of
getting rid of dead or dying blood cells as well as foreign matter such as dust
and asbestos. Red cells remain viable for only about 4 months before they
are removed from the blood and their components recycled in the spleen.
Individual white cells usually only last 18-36 hours before they also are
removed, though some types live as much as a year. The description of
white cells presented here is a simplification. There are actually many
specialized sub-types of them that participate in different ways in our immune
responses.
) are the first responders for our immune system. They seek
out, identify, and bind to alien protein on bacteria, viruses,
and fungi so that they can be removed. Other white cells
(called granulocytes and macrophages ) then arrive to
surround and destroy the alien cells. They also have the function of
getting rid of dead or dying blood cells as well as foreign matter such as dust
and asbestos. Red cells remain viable for only about 4 months before they
are removed from the blood and their components recycled in the spleen.
Individual white cells usually only last 18-36 hours before they also are
removed, though some types live as much as a year. The description of
white cells presented here is a simplification. There are actually many
specialized sub-types of them that participate in different ways in our immune
responses.
Platelets
|
|
|
|
erythrocyte (left), thrombocyte |
Platelets , or thrombocytes , are cell fragments without nuclei that work with blood clotting chemicals at the site of wounds. They do this by adhering to the walls of blood vessels, thereby plugging the rupture in the vascular wall. They also can release coagulating chemicals which cause clots to form in the blood that can plug up narrowed blood vessels. Thirteen different blood clotting factors, in addition to platelets, need to interact for clotting to occur. They do so in a cascading manner, one factor triggering another. Hemophiliacs lack the ability to produce either blood factor 8 or 9.
Platelets are not equally effective in clotting blood throughout the entire day. The body's circadian rhythm system (its internal biological clock) causes the peak of platelet activation in the morning. This is one of the main reasons that strokes and heart attacks are more common in the morning.
Recent research has shown that platelets also help fight infections by releasing proteins that kill invading bacteria and some other microorganisms. In addition, platelets stimulate the immune system. Individual platelets are about 1/3 the size of red cells. They have a lifespan of 9-10 days. Like the red and white blood cells, platelets are produced in bone marrow from stem cells.
Plasma
Plasma is the relatively clear, yellow tinted water (92+%), sugar, fat, protein and salt solution which carries the red cells, white cells, and platelets. Normally, 55% of our blood's volume is made up of plasma. As the heart pumps blood to cells throughout the body, plasma brings nourishment to them and removes the waste products of metabolism. Plasma also contains blood clotting factors, sugars, lipids, vitamins, minerals, hormones, enzymes, antibodies, and other proteins. It is likely that plasma contains some of every protein produced by the body--approximately 500 have been identified in human plasma so far.
Agglutination
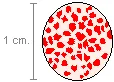
Sometimes when the blood of two people is mixed together, it clumps or forms visible islands in the liquid plasma--the red cells become attached to one another. This is agglutination .
|
|
|
|
|
|
|
|
When different types of blood are mixed within the body, the reaction can be a bursting of the red cells as well as agglutination. Different types of blood are recognized on the molecular level and sometimes rejected by being destroyed and ultimately filtered out by the kidneys in order to expel them from the body along with urine. In the case of a transfusion mistake, there can be so much of the wrong type of blood in the system that it can result in kidney failure and death. This is due to the fact that when the kidneys try to filter the blood, they essentially become clogged as they are overwhelmed and cease being effective filters. Additionally, there is a rapid depletion of blood clotting factors which causes bleeding from every body orifice. In the United States, about 1 in 12,000 units of whole blood transfused is given to the wrong person. Depending on the blood types of the donor and the recipient, this can result in death or no problems at all.
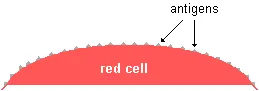
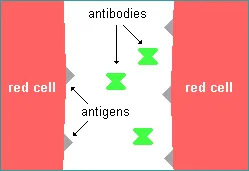
The compositional difference between blood types is in the specific kinds of antigens found on the surface of the red cells. Antigens are relatively large protein molecules that provide the biological signature of an individual's blood type.
|
|
|
|
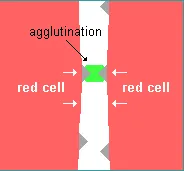
Within blood, there are substances called antibodies which distinguish particular antigens from others, causing bursting or agglutination of the red cells when alien antigens are found. The antibodies bind to the antigens. In the case of agglutination, the antibodies "glue" together the antigens from different red cells thereby sticking the red cells together (as shown below on the right).
|
Antibodies seeking specific antigens |
|
Antibodies agglutinating red cells |
|
|
|
|
|
|
||
As agglutination proceeds, millions of red cells are glued together into clumps. This is not the same thing as clotting. When agglutination occurs, the blood mostly remains liquid. With clotting, however, it does not.
The specific types of antigens on our red blood cells determine our blood types. There are 29 known human blood systems, or groups, for which each of us can be typed. As a result, there are one or more antigens for each of these blood groups. Since many of these blood systems also are found in apes and monkeys, it is likely that they evolved prior to the time that we became a separate species.
Long before the phenomenon of blood antigen-antibody interaction was discovered, surgeons experimented with human transfusions in an attempt to save the lives of patients who were dying from severe blood loss and the resulting shock. The first attempt may have been an English physician during the mid-17th century who infused a wounded soldier with sheep blood. Not surprisingly, the soldier suffered a painful death. The first successful transfusion of human blood to another human was done by a British doctor in 1818 in order to save the life of a woman who was hemorrhaging following childbirth. By the mid 19th century, European and American doctors used transfusions in a last ditch attempt to save soldiers and other patients with horrendous wounds. They usually transferred blood directly from a healthy individual to their patient via a rubber tube with hypodermic needles at each end. This occasionally resulted in success but more often than not killed the recipient. The results seemed to be random. Doctors in the 19th century also experimented with a variety of blood substitutes, including milk, water, and even oils.
It was the discovery of the ABO blood types in 1900 that finally led us to understand how to consistently use transfusions to save lives. Even with this knowledge, however, life threatening reactions still occur in about 1 out of 80,000 transfusions in developed nations.
White Cell Antibodies
The blood type antigen-antibody interaction is one of many similar recognition-rejection phenomena in our bodies. Infectious microorganisms, such as viruses, also carry foreign antigens which stimulate the production of white cell antibodies (lymphocytes) that attack the antigens by binding to them as a way of getting rid of the invading parasites. Once stem cells in our bone marrow produce antibodies to identify a specific alien antigen, we have the ability to produce them more quickly and in larger numbers. This results in the development of a long-term active immunity to future invasions of the same kind of alien antigen. This is the key to successful vaccination for viruses and some other microorganisms that invade our bodies.
White cell antibodies are also responsible for recognizing and rejecting alien body tissues, or, more accurately, the antigens on their cells. This is the main reason that organ transplants were most often unsuccessful in the past until the creation of drugs that can suppress the immune system and thereby prevent organ rejection. The immune system that is responsible is called the human leukocyte antigen (HLA) system. This is by far the most polymorphic of all known human genetic systems--there are more than 100 antigens on tissue cells in humans resulting in approximately 30,000,000 possible HLA genotypes. The chance of two unrelated people having the same HLA genotypes is very slim. Subsequently, HLA incompatibility between organ donors and recipients are common.