Human Chromosomal Abnormalities
Overview
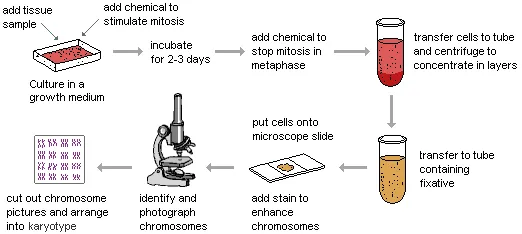
Every human pregnancy that goes to full term in North America and other modern industrialized nations has a small risk (about 2-3%) of serious birth defects. This is the
case even when the mother is young and healthy. However, some pregnancies
are at a higher risk due to a variety of factors. Fortunately, it is now
possible to connect some of the inherited genetic defects to specific chromosome irregularities.
This can be done by examining small tissue samples from adults, children, or
even unborn babies. The samples are cultured to
induce mitosis so that the chromosomes become visible. In this
state, the chromosomes can be photographed. The images are then converted
into a karyotype of the individual from whom the sample was
taken. This involves the precise measurements
of chromatid length ratios and other morphological features so that
they can be placed into homologous pairs.
|
|
|
|
|
|
|
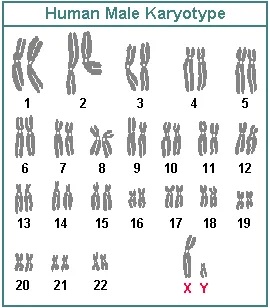
On comparison with a normal karyotype, major abnormalities can be discovered in a suspect sample. Irregular numbers of chromosomes and missing or deformed chromatids are easily observed. Many types of gross chromosomal abnormalities have been connected to specific medical syndromes , including mental retardation.
By sampling embryonic or fetal cells within the uterus of a mother, it is possible to determine whether or not her child will be born with serious genetic problems. More than 80 common types of chromosomal abnormalities are now identifiable by this method. The unborn child's gender can also be determined by noting whether its karyotype includes X and Y sex chromosomes or only X's. Gender is important because of the higher probability of males expressing X-linked traits in their phenotypes.
By this simple examination of karyotypes, it is not possible to discover mutations that occur at the gene level. That is to say, mutations in the DNA molecules that make up chromosomes are not usually detected by this process. Since it is likely that most of the more than 5,000 known genetic disorders are at this lower level, karyotype analysis is limited. However, those disorders that are due to gross chromosomal irregularities are comparatively common and often serious. As a result, karyotype analysis and other associated tests have become important medical tools.
Detection
Karyotyping can be done from blood,
hair, or any other tissue. However, most karyotyping for medical
diagnostic purposes is done on embryonic or fetal cells from unborn babies
still in the uterus. The cells are usually collected by one of two
methods: amniocentesis or chorionic villi
sampling . Preliminary testing is now commonly done with a less invasive ultrasound examination of the fetus within the uterus and an analysis of
specific fetal chemicals in the mother's blood. The goal of all of these tests is to determine whether or not the
baby will be abnormal. This information can be the basis for a decision
to perform an abortion or to prepare
parents for the difficulties of raising a child with serious abnormalities and
health problems.
Amniocentesis
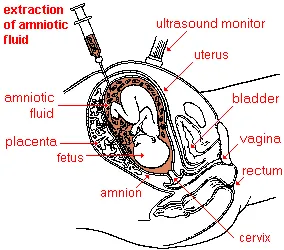
Amniocentesis involves sampling the liquid immediately surrounding a fetus within the amnion (or amniotic sac) as illustrated below. This amniotic fluid is extracted through the mother's abdominal and uterine walls with a hypodermic needle. Local anesthesia is used for this test. The amniotic fluid mostly contains fetal urine but also has millions of fetal skin cells that can be cultured to produce a karyotype. Ultrasound monitoring is commonly used to avoid harming the fetus with the needle. This entire procedure only takes a few minutes in a doctor's office.
|
|
|
|
|
|
|
Extraction of an amniotic fluid sample |
|
|
|
|
|
|
|
Normal human fetus at |
Complete results of amniocentesis tests usually come back from the laboratory in 3-4 weeks. However, determination of gender often can be made in 1-2 days. There is 99+% accuracy in diagnosing Down syndrome and most other gross chromosomal aberrations including neural tube defects such as spina bifida . Amniocentesis can be used to discover the presence of about 400 specific genetic abnormalities in a fetus. These now include some single-gene mutations such as the one that is responsible for the blood disorder beta-thalassemia.
Amniocentesis usually is done from the 15th or 16th week after conception on up to the 20th week. In other words, it is in the 2nd trimester, which is relatively late. Only at this point in a pregnancy is there sufficient amniotic fluid to allow some of it (about 20 cc) to be drawn off without significant danger to the fetus--there is only about .3-.5% risk of the procedure causing a miscarriage. In some cases, amniocentesis is done as early as the 12th-14th week, but the risk of miscarriage is twice as high and the accuracy in detecting neural tube defects is slightly lower.
A variation of the amniocentesis procedure described above involves testing a sample of blood extracted from the umbilical cord. This has an equally high accuracy in diagnosing gross chromosomal abnormalities.
Chorionic Villi Sampling (CVS)
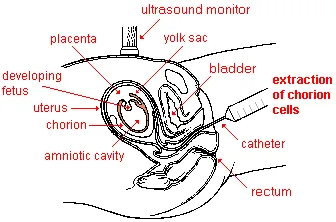
With chorionic villi sampling (or biopsy), a small sample of chorion cells are collected for karyotyping. The chorion is a membrane that develops around an embryo and contributes to the formation of the placenta . Later, as a fetus develops, the chorion fuses with the amnion. The biopsy usually is done by inserting a small flexible plastic tube through the vagina and the cervix into the uterus to draw out a sample of chorion tissue. Alternately, the cells may be extracted with a hypodermic needle through the abdominal and uterine walls, as in the amniocentesis procedure. Local anesthesia also is used for this test. Ultrasound monitoring helps to prevent damage to the unborn child.
|
|
|
Extraction of a sample of chorion cells |
Chorionic villi sampling usually is done beginning in the 10th-12th week of pregnancy. That is still during the 1st trimester when the fetus is quite immature. Final laboratory results usually come back in 2 weeks or less. However, the reliability of those results is less than with amniocentesis. There is approximately 98% accuracy in diagnosing Down syndrome and some other conditions associated with gross chromosomal abnormalities. However, the accuracy in predicting neural tube defects is lower with CVS. The risk of miscarriage is at least 1-3%, or 2-6 times higher than with amniocentesis. As a consequence, chorionic villi sampling is less frequently performed. The risk can be reduced by performing the biopsy no earlier than the 10th week of a pregnancy.
Screening with Maternal
Blood
|
|
|
|
|
|
|
|
A much more routinely done diagnostic procedure for pregnant women is testing their blood for alpha-feto protein and several other chemicals originating from their fetus. This screening is significantly less expensive and has no risk of causing a miscarriage. However, the information gained is less reliable in predicting a chromosomal abnormality. Therefore, positive AFP results are usually followed up by amniocentesis for verification.
Alpha-feto protein is a substance normally produced by the liver of fetuses and is carried in their blood. Some of the fetal blood leaks into the placenta and then into the mother's blood during pregnancy. The AFP, and other diagnostic fetal and maternal chemicals, can be separated from a blood sample taken from the mother's arm. Unusually high or low amounts of AFP relative to the stage of pregnancy indicate that there may be particular kinds of genetic defects. Specifically, it may indicate the likelihood of Down syndrome, neural tube defects, abdominal wall defects, and trisomy 18 .
AFP testing is routinely done in the 14th to 20th week of a pregnancy. If the date of conception has been miscalculated, a false positive test result can occur. A similar error can happen if it is unknown that there are twins, because two fetuses produce more AFP than one.
Other substances of fetal origin found in a mother's blood that are commonly tested for in addition to AFP are the hormones HCG (human chorionic gonadotropin) and unconjugated estriol. The combined testing procedure is referred to as Alpha-fetoprotein Plus or triple screening. Recently, testing for inhibin has also been added to the combined screening. Subsequently, the test is referred to as quadruple or quad screening. The American College of Obstetricians and Gynecologists guidelines now recommend that all pregnant women have triple screening blood tests and ultrasound testing in the first trimester of their pregnancies.
NOTE: Human chorionic gonadotropin is produced by the embryo and later in a pregnancy by the placenta. Unconjugated estriol is a form of estrogen that is made by the liver of the fetus and by the placenta. Inhibin-A is a hormone that plays a part in regulating the menstrual cycle. It is produced normally by the ovaries but also by the placenta during a pregnancy. A newer diagnostic blood test used by some doctors looks for the presence of PAPPA (pregnancy-associated plasma protein A). Still another new test (MaterniT21 LTD) that also involves sampling maternal blood is likely to prove the most reliable for diagnosing Down syndrome. Unlike the other procedures, it does not look for fetal proteins but rather for fetal DNA. Early indications are that it may be 99.1% accurate and have a low false positive rate.
High-resolution Sonogram Screening
The near future of pregnancy screening for birth defects is likely to focus on the new generation of high-resolution ultrasound devices that are now becoming available. They are beginning to be used by doctors who have been specially trained to detect the early anatomical signs associated with some abnormalities. Using this procedure, Down syndrome can be reliably detected in the first trimester of a pregnancy. In addition, it is possible to detect structural defects such as brain cysts and cleft-palates. An advantage of high-resolution sonograms for screening is that they do not increase the risk of miscarriage and can be done early in a pregnancy. In addition, they are relatively inexpensive and quick since there are no samples to be processed in a laboratory. However, it is unlikely in the near future that amniocentesis will stop being considered the gold standard for detecting chromosomal abnormalities.
Screening for Abnormal
DNA and RNA Sequences
Somewhat further in the future will be prenatal blood tests to find and analyze a wide range of abnormal fetal DNA and RNA sequences found in a pregnant woman's blood. Such tests would have the advantages of being relatively inexpensive and noninvasive while providing highly accurate results. One such diagnostic procedure to discover Down syndrome, called MaterniT21, has been developed and is being tested now. Early results indicate that it may be 99.1% accurate with no risk for the fetus. This and other tests may largely replace amniocentesis in the future.